In the realm of healthcare, one of the most critical documents that both patients and providers must understand and acknowledge is the medical consent form. This form serves as a legal and ethical agreement between a patient and their healthcare provider, ensuring that the patient’s informed, voluntary agreement is obtained before any procedure or treatment is conducted.
The purpose of this article is to delve into the significance of medical consent forms, why they are essential, what they should include, how to ensure successful implementation, and some useful tips for both patients and providers.
What is a Medical Consent Form?
A medical consent form is a document that serves as a legal agreement between a patient and their healthcare provider. It is obtained before a medical procedure or treatment is conducted, ensuring that the patient gives their informed, voluntary agreement for the proposed intervention.
This form outlines the nature of the procedure, its risks, potential alternatives, and any other pertinent information that the patient needs to know to make an autonomous decision regarding their healthcare.
Why are Medical Consent Forms Important?
Medical consent forms are crucial for both patients and providers.
For patients, these forms protect their right to make autonomous decisions about their healthcare by ensuring that they have all the necessary information about a procedure before agreeing to it. This protects patients from undergoing treatments or procedures without fully understanding the implications.
For healthcare providers, medical consent forms offer legal protection by documenting that they have fulfilled their ethical and legal obligation to inform the patient before proceeding with any intervention.
Legal Protection
Medical consent forms serve as a form of legal protection for healthcare providers. By obtaining informed consent from patients before conducting a procedure or treatment, providers can mitigate the risk of potential lawsuits or claims of negligence. In the event of a dispute or legal challenge, having a signed medical consent form that outlines the risks and benefits of the intervention can be crucial evidence in defending the provider’s actions. Without proper consent documentation, providers may be vulnerable to legal repercussions.
Ethical Obligation
In addition to legal considerations, medical consent forms fulfill an ethical obligation that healthcare providers have towards their patients. Informed consent is rooted in the principle of respect for patient autonomy, which emphasizes the right of individuals to make decisions about their own healthcare. By engaging patients in the decision-making process and ensuring that they understand the implications of their choices, providers demonstrate a commitment to ethical care delivery and patient-centered practice. Medical consent forms are a tangible manifestation of this ethical obligation.
Risk Management
From a risk management perspective, medical consent forms are an essential tool for healthcare providers to mitigate potential risks associated with procedures or treatments. By informing patients about the risks, benefits, and alternatives of an intervention, providers help patients make informed decisions that align with their preferences and values. This proactive approach to risk management can reduce the likelihood of adverse outcomes, patient dissatisfaction, or misunderstandings about the proposed treatment. Ultimately, medical consent forms contribute to safer and more effective patient care.
Patient Empowerment
Empowering patients to participate in their healthcare decisions is a central tenet of patient-centered care. Medical consent forms play a pivotal role in this empowerment process by providing patients with the information they need to make decisions that align with their values and preferences. When patients are actively involved in the consent process, they are more likely to feel engaged in their care, respected as partners in the healthcare journey, and satisfied with the outcomes of their treatment. Patient empowerment through informed consent promotes better communication, trust, and collaboration between patients and providers.
Documentation and Communication
Another crucial aspect of medical consent forms is their role in documentation and communication within the healthcare setting. By documenting the consent process, including the information provided to the patient, their questions and concerns, and the final agreement, healthcare providers create a comprehensive record of the patient’s involvement in their care. This documentation serves as a communication tool between providers, ensuring that all members of the healthcare team are aware of the patient’s preferences and decisions. Clear communication through medical consent forms enhances care coordination, continuity, and patient safety.
What to Include in a Medical Consent Form?
When creating a medical consent form, it is essential to include specific information to ensure that the patient is adequately informed before giving their consent. Some key elements to include in a medical consent form are: Description of the procedure or treatment, risks and potential complications, alternatives to the proposed intervention, expected outcomes, signature lines for the patient and the healthcare provider, date and time of consent.
Description of the Procedure
The medical consent form should provide a detailed description of the procedure or treatment that the patient is consenting to undergo. This description should be written in clear, non-technical language that the patient can easily understand. The purpose, goals, and steps involved in the procedure should be outlined to give the patient a comprehensive understanding of what to expect. Including information about the duration of the procedure, any special requirements or preparations, and the expected outcomes can help patients make an informed decision about their care.
Risks and Potential Complications
Informed consent requires that patients be made aware of the potential risks and complications associated with a procedure or treatment. The medical consent form should outline the common risks, side effects, and complications that may arise as a result of the intervention. This information helps patients weigh the benefits of the treatment against the potential harms and make a decision that aligns with their values and preferences. Healthcare providers should communicate the risks in a way that is easy to understand, emphasizing the likelihood and severity of each potential complication.
Alternatives to the Proposed Intervention
Patients have the right to know about alternative treatment options or approaches that may be available for their condition. The medical consent form should include information about alternative interventions, including their benefits, risks, and potential outcomes. Healthcare providers should discuss the advantages and disadvantages of each alternative with the patient, allowing them to compare different options and make an informed choice. By presenting alternatives, providers demonstrate a commitment to patient-centered care and shared decision-making.
Expected Outcomes
Patients should have realistic expectations about the outcomes of a procedure or treatment before giving their consent. The medical consent form should provide information about the expected benefits of the intervention, including the goals it aims to achieve and the improvements in health or quality of life that can be anticipated. By setting realistic expectations, patients can make informed decisions about their care and understand what they can expect from the treatment. Healthcare providers should be transparent about the limitations of the intervention and any uncertainties regarding its efficacy.
Signature Lines and Consent Date
To formalize the consent process, the medical consent form should include signature lines for both the patient and the healthcare provider. The patient’s signature indicates that they have understood the information provided, had the opportunity to ask questions, and voluntarily agree to undergo the specified procedure. The healthcare provider’s signature signifies that they have discussed the relevant information with the patient, answered any questions, and obtained consent in accordance with ethical and legal standards. Including the date and time of consent helps to document when the agreement was made and ensures clarity about the timing of the intervention.
Additional Information
Depending on the nature of the procedure or treatment, the medical consent form may need to include additional information to ensure that the patient is fully informed. This could include details about potential costs or financial implications, instructions for post-procedure care, information about follow-up appointments or monitoring, and any other relevant details that the patient should be aware of before giving their consent. Providing comprehensive information in the consent form helps to set clear expectations and ensures that the patient is prepared for all aspects of their care.
How to Obtain Medical Consent
Obtaining medical consent involves a thorough process of patient education and communication. Healthcare providers should take the time to explain the proposed procedure or treatment in simple terms, ensuring that the patient understands all aspects of the intervention. It is crucial to answer any questions the patient may have and address any concerns before asking for their consent. Written consent should be obtained before proceeding with the medical intervention.
Effective Communication
Effective communication is the cornerstone of obtaining medical consent from patients. Healthcare providers should strive to communicate clearly, using language that is easy for patients to understand. Avoiding medical jargon and complex terminology can help patients grasp the information presented and make informed decisions about their care. Providers should encourage open dialogue, actively listen to patients’ concerns, and provide additional explanations or resources as needed to ensure that the patient feels fully informed and empowered to consent.
Educational Materials
In addition to verbal communication, healthcare providers can use educational materials to support the consent process. Providing written information about the procedure, including brochures, pamphlets, or fact sheets, can help reinforce the details discussed during the consent conversation. Visual aids, such as diagrams or videos, can further enhance patient understanding and facilitate discussions about the procedure. By using a combination of verbal explanations and written materials, providers can cater to different learning styles and ensure that patients receive comprehensive information.
Question and Answer Session
Encouraging patients to ask questions and engage in a dialogue about their care is essential for obtaining informed consent. Healthcare providers should create a safe and welcoming environment where patients feel comfortable expressing their concerns, seeking clarification, and discussing their preferences. Hosting a question and answer session allows patients to voice any uncertainties, fears, or doubts they may have about the procedure, enabling providers to address these issues and ensure that the patient is fully informed before giving their consent.
Shared Decision-Making
Shared decision-making is a collaborative approach to healthcare that involves patients and providers working together to make decisions about treatment. When obtaining medical consent, healthcare providers should engage patients in the decision-making process, discussing the options available, presenting the pros and cons of each choice, and considering the patient’s values and preferences. By involving patients in the decision-making process, providers can ensure that the treatment plan aligns with the patient’s goals and priorities, leading to greater satisfaction and adherence to care recommendations.
Respecting Patient Autonomy
Respecting patient autonomy is a fundamental principle in healthcare that underpins the concept of informed consent. Healthcare providers should recognize and uphold the patient’s right to make decisions about their own care, including the option to accept or refuse treatment. Respecting patient autonomy involves providing patients with the information they need to make informed decisions, supporting their choices, and ensuring that their preferences are central to the care planning process. By respecting patient autonomy, providers demonstrate a commitment to patient-centered care and ethical practice.
Tips for Successful Medical Consent
Ensuring successful medical consent involves effective communication and patient engagement. Some tips for healthcare providers to obtain successful medical consent are: Use plain language and avoid medical jargon, provide written information about the procedure, encourage patients to ask questions and address any concerns, offer additional resources or support for decision-making, and document the consent process thoroughly in the patient’s medical record.
Use Plain Language
When discussing medical procedures or treatments with patients, healthcare providers should use plain language that is easy for patients to understand. Avoiding complex medical terminology or jargon can help patients grasp the information presented and make informed decisions about their care. Using simple explanations, analogies, and real-life examples can enhance patient understanding and facilitate meaningful conversations about the proposed intervention. By using plain language, providers can ensure that patients feel confident and empowered to participate in the consent process.
Provide Written Information
In addition to verbal explanations, providing written information about the procedure can reinforce key details and help patients retain important information. Healthcare providers can offer brochures, handouts, or fact sheets that outline the procedure, its risks and benefits, potential alternatives, and expected outcomes. Written materials serve as a reference for patients to review at their own pace, share with family members, or consult after the consent conversation. By providing written information, providers support patient education and empower patients to make well-informed decisions.
Encourage Questions and Concerns
Patients may have questions, concerns, or uncertainties about a proposed procedure, and healthcare providers need to create a supportive environment where these issues can be addressed. Encouraging patients to ask questions, seek clarification, and voice their concerns can help providers identify and mitigate any barriers to informed consent. Patients should feel comfortable expressing their doubts or fears, knowing that their provider is available to listen, provide information, and offer reassurance. By encouraging open communication, providers foster trust and collaboration with their patients.
Offer Additional Resources
In some cases, patients may benefit from additional resources or support to aid their decision-making process. Healthcare providers can offer supplemental materials, such as online resources, educational videos, or contact information for patient advocacy organizations, to help patients gather more information about their condition or treatment options. Referring patients to support groups, counseling services, or second opinions can also enhance their understanding and confidence in making decisions about their care. By offering additional resources, providers demonstrate a commitment to comprehensive patient care.
Thorough Documentation
Documenting the consent process thoroughly in the patient’s medical record is essential for ensuring that the patient’s agreement is well-documented and legally valid. Healthcare providers should record the details of the consent conversation, including the information provided to the patient, their questions and concerns, and the final agreement reached. Documenting the consent process helps to demonstrate that the patient was adequately informed, actively engaged in the decision-making process, and voluntarily agreed to the proposed intervention. By maintaining accurate records, providers uphold ethical standards and legal requirements related to informed consent.
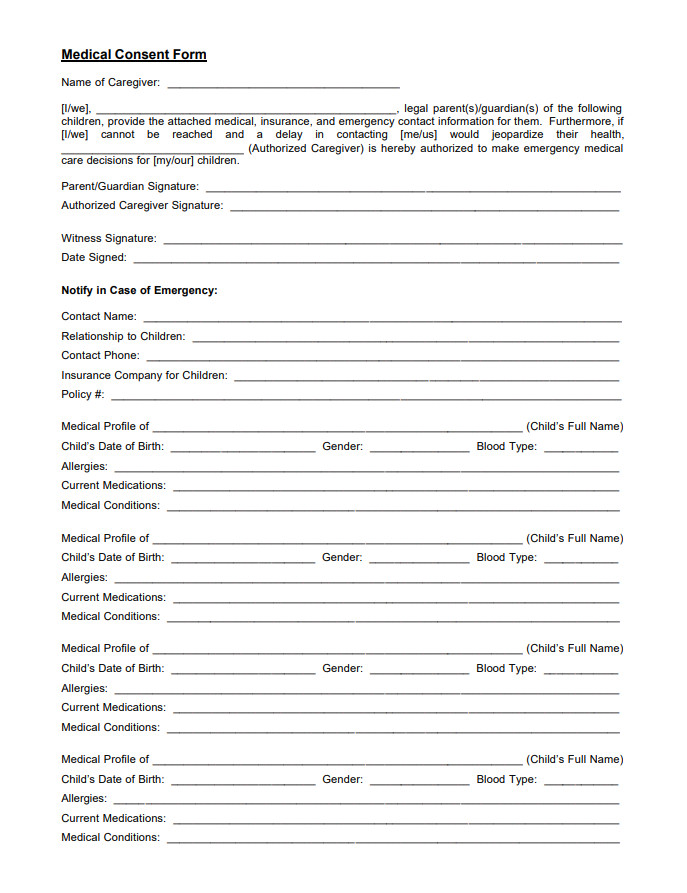
Medical Consent Form – DOWNLOAD
- Free Notary Acknowledgement Form Template - February 27, 2026
- Free Printable Nutrition Chart Template - February 26, 2026
- Free Student Reference Letter Template (Word) - February 22, 2026