What Is A Mental Status Exam?
A Mental Status Exam (MSE) is a structured assessment tool used by healthcare professionals to evaluate an individual’s current mental state. It involves a thorough examination of the patient’s cognitive abilities, emotional functioning, and behavior.
The MSE provides valuable insights into the patient’s mental health and helps clinicians identify potential areas of concern or impairment that may require further evaluation or intervention.
What Is Included In A Mental Status Exam?
When healthcare providers perform a Mental Status Exam, they examine various aspects of the patient’s mental functioning to gain a comprehensive understanding of their current state. The components of an MSE typically include:
Cognitive Functioning
Assessing cognitive functioning involves evaluating the patient’s ability to process information, remember details, solve problems, and communicate effectively. During this part of the exam, healthcare providers may ask the patient to perform tasks that require attention, memory, and executive function. By assessing cognitive functioning, clinicians can identify any cognitive deficits that may be impacting the patient’s daily functioning and quality of life.
For example, testing memory recall may involve asking the patient to remember a list of words or a series of numbers after a short delay. Evaluating problem-solving skills may involve presenting the patient with a complex scenario and asking them to generate potential solutions. By observing the patient’s performance on these tasks, healthcare providers can gain insights into their cognitive strengths and weaknesses.
Emotional State and Mood
Observing the patient’s emotional state and mood is another crucial component of the MSE. Healthcare providers pay attention to the patient’s overall affect, which includes their facial expressions, tone of voice, and body language. By assessing the patient’s emotional responses to different stimuli and situations, clinicians can determine if there are any significant mood disturbances, such as depression, anxiety, or mania.
During this part of the exam, healthcare providers may ask the patient about their current mood, feelings of sadness or hopelessness, and any changes in appetite or sleep patterns. By exploring the patient’s emotional experiences, clinicians can gain a deeper understanding of their mental well-being and emotional functioning. This information is essential for diagnosing and treating mood disorders effectively.
Behavioral Observations
Noting any unusual behaviors or motor abnormalities is another important aspect of the MSE. Healthcare providers observe the patient’s behavior during the exam to identify any signs of agitation, restlessness, impulsivity, or other behavioral changes. These observations can provide valuable insights into the patient’s mental state and help clinicians assess their level of functioning.
For example, healthcare providers may note if the patient exhibits repetitive movements, speaks rapidly or incoherently, or displays signs of paranoia or agitation. These behavioral observations can indicate underlying mental health conditions, such as psychosis, substance use disorder, or neurocognitive impairment. By documenting these behaviors during the MSE, clinicians can make more accurate diagnoses and recommend appropriate interventions.
Thought Content and Perceptual Disturbances
Evaluating the patient’s thought content and perceptual disturbances is essential for a comprehensive MSE. Healthcare providers assess the patient’s thoughts, beliefs, and perceptions to determine if there are any distortions or abnormalities present. This part of the exam helps clinicians identify potential delusions, hallucinations, or other psychotic symptoms that may indicate a severe mental health condition.
During the assessment, healthcare providers may ask the patient about their beliefs, fears, and experiences to gain insight into their thought processes. They may also inquire about any auditory or visual hallucinations the patient may be experiencing. By exploring these aspects of the patient’s mental state, clinicians can gather valuable information to guide their diagnostic and treatment decisions.
Insight and Judgment
Assessing the patient’s insight and judgment is an important component of the MSE. Insight refers to the patient’s awareness of their mental health condition and its implications for their daily life. Judgment involves the patient’s ability to make sound decisions and understand the consequences of their actions. By evaluating insight and judgment, healthcare providers can assess the patient’s level of self-awareness and capacity for decision-making.
During this part of the exam, clinicians may ask the patient about their understanding of their diagnosis, treatment recommendations, and the impact of their mental health on their relationships and responsibilities. By exploring the patient’s insight and judgment, healthcare providers can determine if the individual is capable of making informed decisions about their care and managing their mental health effectively.
When Do Healthcare Providers Perform A Mental Status Exam?
Healthcare providers may conduct a Mental Status Exam in a variety of clinical settings to assess an individual’s mental state and determine the presence of any mental health conditions. The timing and frequency of the MSE may vary based on the patient’s needs and the healthcare provider’s clinical judgment. Some common situations in which healthcare providers perform a Mental Status Exam include:
Diagnostic Assessment
One of the primary reasons healthcare providers conduct a Mental Status Exam is to aid in the diagnostic assessment of mental health conditions. When a patient presents with symptoms that suggest a possible mental health disorder, clinicians may perform an MSE to gather additional information and confirm a diagnosis. The findings from the exam help healthcare providers differentiate between various conditions and develop a treatment plan tailored to the individual’s specific needs.
For example, if a patient exhibits symptoms of depression, such as persistent sadness, loss of interest in activities, and changes in appetite or sleep patterns, a thorough MSE can help confirm the diagnosis and rule out other possible causes of the symptoms. By carefully evaluating the patient’s cognitive abilities, emotional state, and behavior, clinicians can make a more accurate diagnosis and recommend appropriate interventions.
Treatment Planning
Healthcare providers also perform Mental Status Exams to inform treatment planning for individuals with mental health conditions. The information gathered during the exam helps clinicians tailor treatment interventions to address the patient’s specific needs and goals. By understanding the patient’s cognitive functioning, emotional state, and behavioral patterns, healthcare providers can recommend targeted therapies and medications to improve the individual’s mental well-being.
For instance, if the MSE reveals significant cognitive deficits in a patient with dementia, healthcare providers may recommend cognitive rehabilitation strategies to enhance memory and executive function. If
the exam uncovers severe anxiety symptoms, clinicians may suggest a combination of therapy and medication to manage anxiety and improve quality of life. By utilizing the results of the MSE to guide treatment planning, healthcare providers can offer more effective and personalized care to their patients.
Monitoring Progress
In addition to aiding in diagnosis and treatment planning, healthcare providers perform follow-up Mental Status Exams to monitor a patient’s progress over time. Regularly assessing the patient’s mental state allows clinicians to track changes in symptoms, evaluate the effectiveness of treatment interventions, and make adjustments as needed. Monitoring progress through MSEs helps healthcare providers ensure that the patient is responding well to treatment and experiencing improvements in their mental health.
For example, if a patient with depression undergoes treatment with therapy and medication, conducting periodic MSEs can help healthcare providers assess changes in mood, cognitive function, and overall well-being. By comparing the results of follow-up MSEs to the initial assessment, clinicians can determine if the treatment is effective and make modifications to optimize the patient’s outcomes.
Emergency Situations
In emergencies or crises, healthcare providers may perform a Mental Status Exam to quickly assess an individual’s mental state and determine if immediate intervention is needed. For example, if a patient presents to the emergency room with symptoms of acute psychosis, healthcare providers may conduct an MSE to evaluate the severity of the symptoms and determine the appropriate course of action. The findings from the exam help guide decisions about hospitalization, treatment options, and ongoing care for the individual.
During emergency Mental Status Exams, healthcare providers prioritize the safety and well-being of the patient while gathering essential information to inform clinical decision-making. By conducting a thorough assessment of the patient’s mental state, clinicians can provide timely and appropriate care to individuals in crisis situations.
How To Examine Mental Status?
Conducting a thorough Mental Status Exam requires healthcare providers to follow a systematic and comprehensive approach to assessing the patient’s mental state. The exam typically involves a combination of observational techniques, interview questions, and standardized assessment tools to gather information across various domains of mental functioning. Healthcare providers may use the following strategies to examine the patient’s mental status:
Observation
One of the key components of an MSE is observation. Healthcare providers carefully observe the patient’s appearance, behavior, speech patterns, and interactions during the exam to gather valuable information about their mental state. Observational skills allow clinicians to assess the patient’s overall demeanor, level of distress, and any unusual behaviors that may indicate underlying mental health concerns.
For example, healthcare providers may note if the patient appears disheveled, exhibits signs of agitation, or demonstrates poor eye contact during the exam. These observations can provide important insights into the patient’s emotional state, cognitive function, and level of engagement with the clinician. By paying attention to these visual cues, healthcare providers can gather valuable information to inform their assessment and treatment recommendations.
Interviews
Conducting interviews is another essential aspect of the MSE. Healthcare providers use structured interview questions to gather information about the patient’s thoughts, feelings, perceptions, and behaviors. By engaging in dialogue with the patient, clinicians can explore specific areas of concern, assess symptoms, and gain a deeper understanding of the individual’s mental health and well-being.
During the interview portion of the MSE, healthcare providers may ask the patient about their current mood, recent experiences, any changes in sleep or appetite, and thoughts of self-harm or suicide. These questions help clinicians evaluate the patient’s emotional state, cognitive function, and risk factors for mental health issues. By actively listening to the patient’s responses and asking probing questions, healthcare providers can gather detailed information to guide their assessment and treatment decisions.
Standardized Assessments
Using standardized assessment tools is another valuable strategy for examining mental status. Healthcare providers may administer validated tests and scales to measure specific aspects of cognitive functioning, mood, and behavior. These tools provide objective data that can help healthcare providers evaluate the patient’s mental state, track changes over time, and make informed clinical decisions.
For example, healthcare providers may use standardized scales to assess cognitive abilities, such as memory, attention, and executive function. These assessments can help clinicians identify cognitive deficits, track changes in cognitive function, and monitor the effectiveness of interventions. By utilizing standardized assessment tools, healthcare providers can gather quantitative data to supplement their clinical observations and enhance the accuracy of their diagnostic and treatment decisions.
Collaboration and Communication
Collaboration and communication are essential components of conducting a thorough Mental Status Exam. Healthcare providers work collaboratively with the patient, their families, and other members of the healthcare team to gather information, share observations, and develop a comprehensive understanding of the patient’s mental state. Effective communication ensures that all stakeholders are informed and involved in the assessment process.
For example, healthcare providers may consult with other specialists, such as psychiatrists, psychologists, or social workers, to gather additional insights and perspectives on the patient’s mental health. Collaborating with members of the healthcare team allows clinicians to consider multiple viewpoints, share expertise, and develop a holistic approach to care. By fostering open communication and collaboration, healthcare providers can ensure that the patient receives a comprehensive and coordinated mental health assessment and treatment.
Cultural Considerations
When examining mental status, healthcare providers must consider the cultural background and beliefs of the patient. Cultural factors can influence the expression of mental health symptoms, attitudes toward treatment, and help-seeking behaviors. Healthcare providers should approach the MSE with cultural sensitivity and awareness to ensure that the assessment is respectful and inclusive of the patient’s cultural values and practices.
For example, some cultures may stigmatize mental health issues or have specific beliefs about the causes of mental illness. Healthcare providers should be mindful of these cultural perspectives and adapt their approach to the MSE accordingly. By considering cultural factors, healthcare providers can build trust, foster rapport, and enhance the effectiveness of the assessment process. Cultural competence is essential for providing patient-centered care and promoting positive mental health outcomes.
The Impact of Mental Status Exam on Patient Care
Overall, the Mental Status Exam plays a critical role in mental health assessment and patient care. By systematically evaluating the patient’s cognitive abilities, emotional state, and behavior, healthcare providers can gain valuable insights into the individual’s mental functioning and well-being. The information gathered during the MSE informs diagnostic decisions, treatment planning, and ongoing monitoring of the patient’s progress.
Through collaboration, communication, and cultural sensitivity, healthcare providers can conduct a comprehensive and personalized Mental Status Exam that addresses the unique needs of each individual. By using a combination of observation, interviews, standardized assessments, and cultural considerations, clinicians can gather detailed information to guide their clinical decisions and provide high-quality care to their patients.
Ultimately, the Mental Status Exam is a valuable tool that helps healthcare providers better understand their patients’ mental health, identify areas of concern, and develop tailored treatment plans. By incorporating the MSE into routine clinical practice, healthcare providers can enhance the quality of mental health assessment and improve outcomes for individuals experiencing mental health challenges.
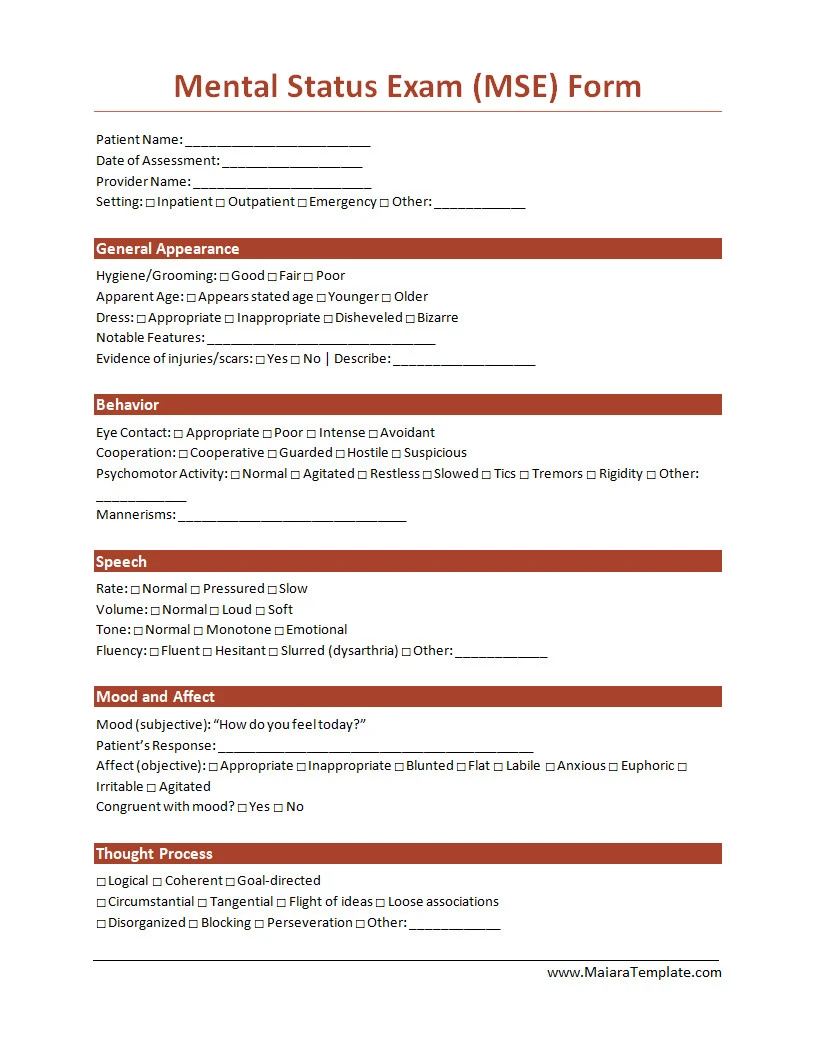
Mental Status Exam Template – DOWNLOAD
- Free Nursing Student Resume Template (Word) - March 1, 2026
- Free Notary Acknowledgement Form Template - February 27, 2026
- Free Printable Nutrition Chart Template - February 26, 2026